Abstract
Editorial Note
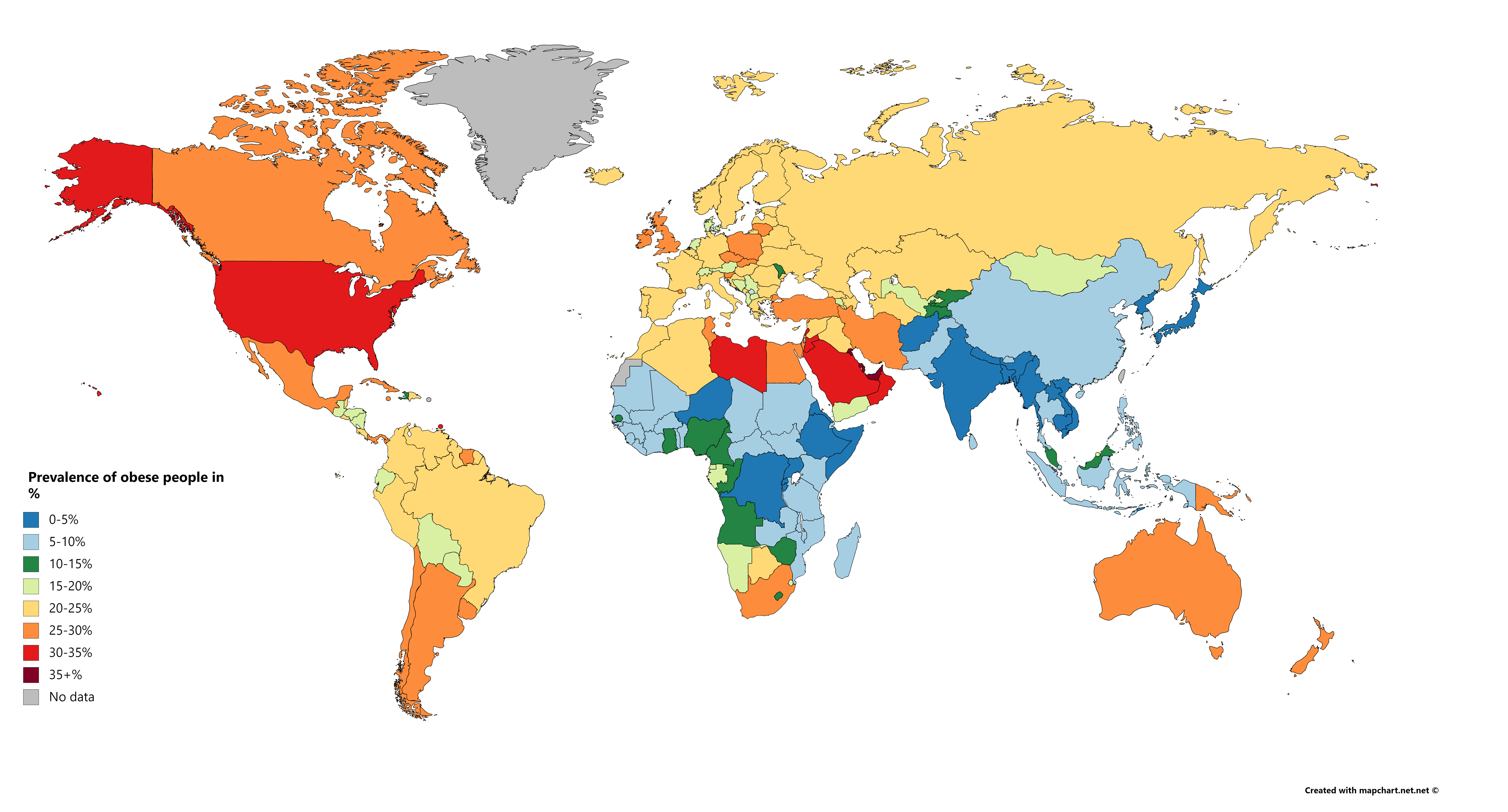
Type 2 diabetes mellitus and hypertension are the most common comorbidities in patients with coronavirus infections. Emerging evidence demonstrates an important direct metabolic and endocrine mechanistic link to the viral disease process. Metabolic syndrome (METS) is a common denominator to these comorbidities and includes insulin resistance, dyslipidaemia, central obesity and hypertension, which are risk factors for the development of type 2 diabetes and cardiovascular diseases. In 2017, it was estimated that METS affected 20% of the North American population, 25% of the European population and approximately 15% of the Chinese population. In this scenario, the relationship between METS and its comorbidities that aggravate the COVID-19 prognosis cannot be ignored. Also, its presence in different ethnicities and continents places METS as an important risk factor for COVID-19. The authors offer their scientific and epidemiological perspective on this emerging association and urge an international awareness of its devastating consequences among certain populations. This article welcomes debate among scientists, policymakers and wider community leaders. The authors urge clinicians to encourage thorough metabolic control for all patients at risk of COVID-19. (a,b) The Physician welcomes contributions from interested scientists, policymakers and patient representative organisations to continue this discourse.
References
a. Bornstein, S.R., Dalan, R., Hopkins, D. et al. Endocrine and metabolic link to coronavirus infection. Nat Rev Endocrinol 16, 297–298 (2020). https://doi.org/10.1038/s41574-020-0353-9
b. Costa, F.F., Rosário, W.R., Farias, A.C.R., de Souza, R.G., Gondim, R.S.D., Barroso,W.A. Metabolic syndrome and COVID-19: An update on the associated comorbidities and proposed therapies. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 2020 14(5), 809-814, https://doi.org/10.1016/j.dsx.2020.06.016
Harrison, E., Docherty, A., Semple, C. (2020) Investigating associations between ethnicity and outcome from COVID-19 UK Gov CO-CIN ePub 25/04/2020 (accessed 7.7.2020) https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/886433/s0238-co-cin-report-ethnicity-outcomes-250420-sage29.pdf
Unnikrishnan, R., Anjana, R.M., Mohan, V. (2014) Diabetes in South Asians: Is the Phenotype Different? Diabetes 63 (1) 53-55; DOI: 10.2337/db13-1592
Chauhan, S., Tamber Aeri, B. (2013) Prevalence of cardiovascular disease in India and its economic impact- A review. Int J Scien Res Publ, 3(10) http://www.ijsrp.org/research-paper-1013/ijsrp-p2234.pdf (accessed 7.7.20)
Andersen CJ, Murphy KE, Fernandez ML. (2016) Impact of Obesity and Metabolic Syndrome on Immunity. Adv Nutr. 7(1):66-75. doi:10.3945/an.115.010207
Arau´ jo, J., Cai, J., Stevens, J. (2019) Prevalence of Optimal Metabolic Health in American Adults: National Health and Nutrition Examination Survey 2009–2016. Metabolic syndrome and related disorders. 17(1) Mary Ann Liebert, Inc. Pp. 46–52 DOI: 10.1089/met.2018.0105
Kelly, C.T., Mansoor, J., Dohm, G.L., Chapman III, W.H.H., Pender IV, J.R., Pories, W.J. (2014) Hyperinsulinemic syndrome: The metabolic syndrome is broader than you think. Surgery 156 (2); 405-411 https://doi.org/10.1016/j.surg.2014.04.028
Stefan, N., Schick, F., UlrichHaring, H. (2017) Causes, Characteristics, and Consequences of Metabolically Unhealthy Normal Weight in Humans. Cell Metabolism 26 (2) 292-300 https://doi.org/10.1016/j.cmet.2017.07.008
Joshi P, Islam S, Pais P, et al. Risk Factors for Early Myocardial Infarction in South Asians Compared With Individuals in Other Countries. JAMA. 2007;297(3):286–294. doi:10.1001/jama.297.3.286
Dasgupta R, Pillai R, Kumar R, Arora NK. Sugar, salt, fat, and chronic disease epidemic in India: is there need for policy interventions?. Indian J Community Med. 2015;40(2):71-74. doi:10.4103/0970-0218.153858
Iliodromiti S, Ghouri N, Celis-Morales CA, Sattar N, Lumsden MA, Gill JM. Should Physical Activity Recommendations for South Asian Adults Be Ethnicity-Specific? Evidence from a Cross-Sectional Study of South Asian and White European Men and Women. PLoS One. 2016;11(8): doi:10.1371/journal.pone.0160024
Patel, J.V., Chackathayil, J., Hughes, E.A., Webster, C., Lip, G.Y.H., Gill, P.S. (2012) Vitamin D deficiency amongst minority ethnic groups in the UK: a cross sectional study. Int J Cardiol 167 (5) 2172-2176 https://doi.org/10.1016/j.ijcard.2012.05.081
Hu T, Mills KT, Yao L, et al. (2012) Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: a meta-analysis of randomized controlled clinical trials. Am J Epidemiol. 176 (Suppl 7):S44-S54 doi:10.1093/aje/kws264
Zhu L, She ZG, Cheng X, et al. (2020) Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes. Cell Metab. 31(6):1068-1077.e3. doi:10.1016/j.cmet.2020.04.021
Hyde PN, Sapper TN, Crabtree CD, et al. (2019) Dietary carbohydrate restriction improves metabolic syndrome independent of weight loss. JCI Insight. 4(12): doi:10.1172/jci.insight.128308
Berwick DM. The Moral Determinants of Health. JAMA. Published online June 12, 2020. doi:10.1001/jama.2020.11129

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright (c) 2020 Array